Over 6½ years ago, KFF Health News and NPR kicked off “Bill of the Month,” a crowdsourced investigation highlighting the impact of medical bills on patients.
The goal was to understand how the U.S. health care system generates outsize bills and to empower patients with strategies to avoid them. We asked readers and listeners to submit their bills — and they kept coming. “Bill of the Month” has received nearly 10,000 submissions, each a picture of a health system’s dysfunction and the financial burden it places on the patients.
Since 2018, we have analyzed bills totaling almost $6.3 million — including nearly $2.8 million that patients were expected to pay out-of-pocket.
Cited at statehouses and the U.S. Capitol, the series has led to changes in health policy. Two patients featured by “Bill of the Month” were invited to the White House in 2019 to discuss their surprise bills: Elizabeth Moreno’s $18,000 urine test and Drew Calver’s $109,000 heart attack. In 2020, Congress passed the federal No Surprises Act, shielding patients from most out-of-network bills in emergencies, among other protections.
 After Elizabeth Moreno was charged nearly $18,000 for a urine test, she and her father, Paul Davis, sent her surprise bill to “Bill of the Month” — and took their story all the way to the White House. Congress later passed a law against surprise billing.(Julia Robinson for KFF Health News)
After Elizabeth Moreno was charged nearly $18,000 for a urine test, she and her father, Paul Davis, sent her surprise bill to “Bill of the Month” — and took their story all the way to the White House. Congress later passed a law against surprise billing.(Julia Robinson for KFF Health News)Last year, the Biden administration announced plans to lower health costs that included targeting a loophole that allowed health providers to evade the surprise-billing law — a problem first identified by “Bill of the Month.”
Many patients submitted high prescription drug bills. In treatment for prostate cancer, Paul Hinds was billed nearly $74,000 for two shots of an old drug called Lupron, which can cost just a couple of hundred dollars overseas.
Now, the federal government has identified Lupron as one of the medicines that has seen its price rise faster than inflation — meaning its manufacturer owes rebates to Medicare under President Joe Biden’s 2022 Inflation Reduction Act.
The law also authorized the Biden administration to begin negotiating the price of specified drugs for Medicare patients, who now benefit from a cap on the price of insulin.
“Bill of the Month” has helped many patients and readers get their medical bills reduced or forgiven. Roughly 1 in 3 bills were resolved for patients by the time their features were published.
Bisi Bennett was charged $550,124 after her son was in a neonatal intensive care unit for nearly two months — despite having insurance. In a recent interview, nearly three years after her bill was investigated by “Bill of the Month,” she said she initially thought resolving the bill would be simple.
 Despite having insurance, Bisi Bennett was charged $550,124 after her son was in the NICU for nearly two months. She thought resolving the bill would be simple, but the debt hung over her — until a reporter started making calls. “They somehow miraculously figured out how to bill the right parties and get it sorted out,” she says.(Zack Wittman for KFF Health News)
Despite having insurance, Bisi Bennett was charged $550,124 after her son was in the NICU for nearly two months. She thought resolving the bill would be simple, but the debt hung over her — until a reporter started making calls. “They somehow miraculously figured out how to bill the right parties and get it sorted out,” she says.(Zack Wittman for KFF Health News)“Nine months later, 10 months later, I was still fighting with them,” she said. “I really did feel like it kind of robbed me a little bit of the joy of the first months of motherhood.”
Once a reporter started making calls, Bennett said, “they somehow miraculously figured out how to bill the right parties and get it sorted out.”
But relief from individual bills is one thing; patients say bigger solutions are needed for what ails our health system. “This isn’t just about my bill,” Calver said in 2018, when his nearly $109,000 bill was reduced to $332 after being investigated by “Bill of the Month.” “I don’t feel any consumer should have to go through this.”
Email Sign-Up
Subscribe to KFF Health News' free Morning Briefing.
The Takeaways
The “Bill of the Month” mantra is: If the bill is unexpected or seems off, don’t write the check. Each installment offered directions to navigate health care’s rough financial waters.
Some bills memorably illustrated the absurdity of a system that turns ordinary mishaps into extraordinary revenues. After 3-year-old Lucy Branson got a Polly Pocket doll shoe stuck up her nose, her family was charged about $2,659 for an ER doctor to fish it out with forceps — essentially a long pair of tweezers.
Here are some of the most important lessons — and some patients who offered their experiences to teach them:
- Before scheduling services, ask if a provider is in-network — then read waiting-room forms closely. Feeling sick and unable to rule out covid-19, Elyse Greenblatt booked a telemedicine appointment. But her in-network doctor’s office paired her with an out-of-network doctor — and said she’d signed a consent form. Her insurer declined to pay a penny of the $660 bill.
- Ask for an itemized bill, and question charges that don’t make sense. Eloise Reynolds paid her husband’s final hospital bill after he died from colon cancer. A year later, she received a second bill for his stay. Reynolds requested an itemized bill — and using a yardstick as a straight edge, went line by line to sort out why the hospital said she owed nearly $1,100 more. The balance was eventually deemed a “clerical error” and eliminated.
- Beware ambulances. The landmark No Surprises Act protected patients from many surprise bills in emergencies, but it does not apply to ground ambulances, which are unlikely to contract with insurance and thus might bill willy-nilly. When Peggy Dula was in a car accident, she was picked up by a fire department ambulance that was out-of-network. Though she wasn’t terribly hurt, her ride generated a $3,606 charge, and — after her insurance paid an amount it deemed “reasonable and customary” — she owed around $2,711.
- Location Matters, Part 1: Any intervention or test done in a hospital is likely to cost more than elsewhere. After her first prenatal checkup, Reesha Ahmed had her blood drawn for routine tests by a hospital lab. The bill: $9,520. Ahmed, who had a miscarriage, owed $2,390.
- Location Matters, Part 2: Doctors’ offices can be reclassified as hospital facilities if they’re purchased by a hospital system — and then add on hospital facility fees. Kyunghee Lee, a retired seamstress, went to her doctor for regular injections to treat arthritis for a copay of about $30. Then the office moved one floor up — and her bill changed: Newly designated as taking place in “a hospital-based setting,” one visit was billed at $1,394, including a facility fee listed as “operating room services.” Lee owed about $355.
- Location Matters, Part 3: Some free-standing emergency rooms may look like urgent care centers but come with ER charges. Tieqiao Zhang believed he was visiting urgent care when he sought treatment for a kidney stone at a facility called an “urgent care emergency center.” He went there twice and, both times, was given IV hydration and painkillers, then sent home. The visits yielded a bill of $19,543, including a $500 copay for each visit to what was actually a free-standing ER.
- Sometimes it can pay to pay cash. Dani Yuengling needed a breast biopsy after a concerning mammogram. The hospital’s online price calculator listed a price of about $1,400 for those without insurance. So she was shocked to see her own bill, paid using insurance, was almost $18,000, of which she owed more than $5,000 under the terms of her high-deductible plan.
 Any intervention or test done in a hospital is likely to cost more than elsewhere. After her first prenatal checkup, Reesha Ahmed had her blood drawn for routine tests by a hospital lab. The bill: $9,520. Ahmed, who had a miscarriage, owed $2,390.(Nitashia Johnson for KFF Health News)
Any intervention or test done in a hospital is likely to cost more than elsewhere. After her first prenatal checkup, Reesha Ahmed had her blood drawn for routine tests by a hospital lab. The bill: $9,520. Ahmed, who had a miscarriage, owed $2,390.(Nitashia Johnson for KFF Health News)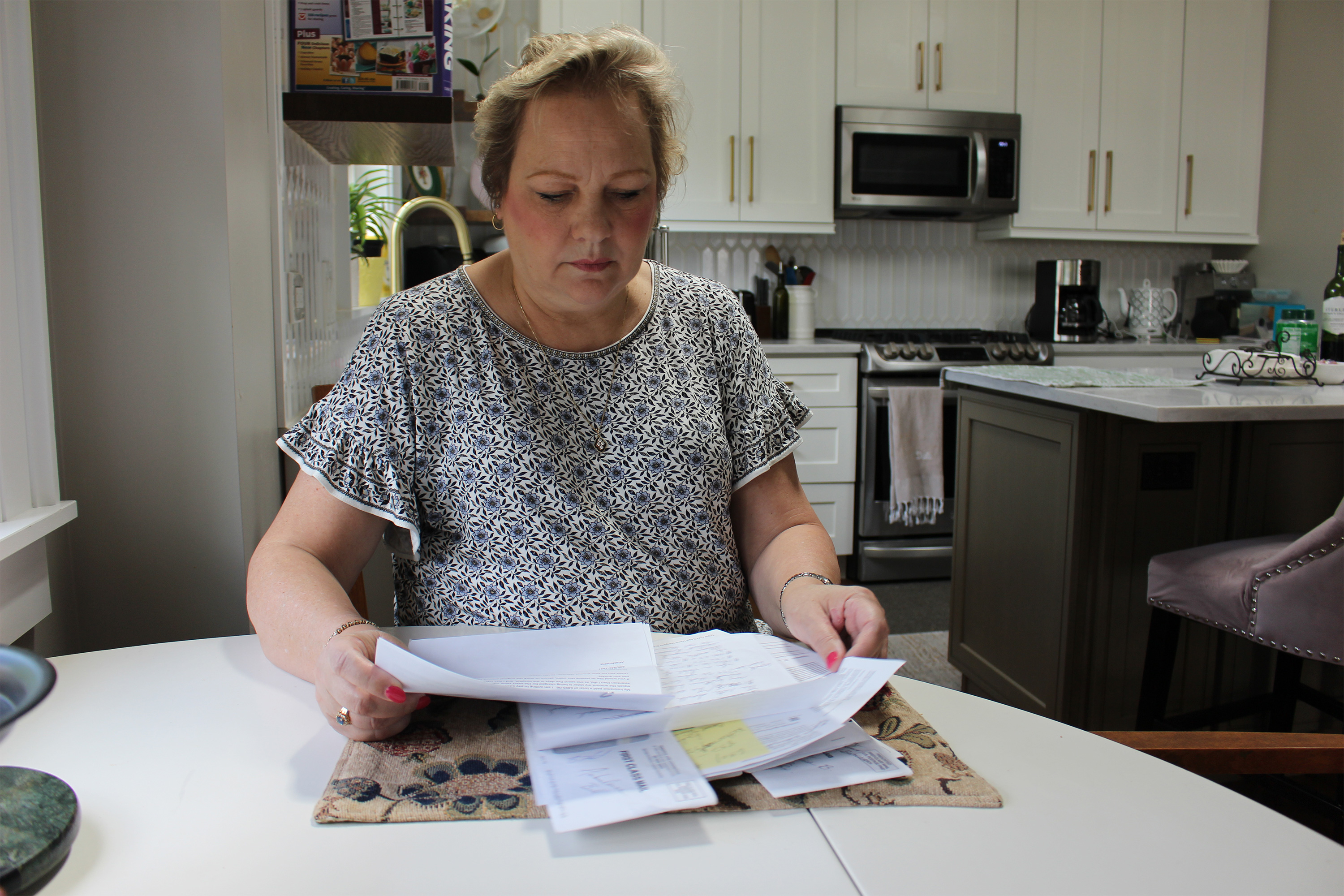 Surprise-billing protections do not apply to ground ambulances. When Peggy Dula was in a car accident, she was picked up by a fire department ambulance. After her insurance paid an amount it deemed “reasonable and customary,” she owed around $2,711.(Bram Sable-Smith/KFF Health News)
Surprise-billing protections do not apply to ground ambulances. When Peggy Dula was in a car accident, she was picked up by a fire department ambulance. After her insurance paid an amount it deemed “reasonable and customary,” she owed around $2,711.(Bram Sable-Smith/KFF Health News) Some free-standing emergency rooms may look like urgent care centers but come with ER charges. Tieqiao Zhang believed he was visiting urgent care when he twice sought treatment for a kidney stone at a facility called an “urgent care emergency center.” The visits yielded a $19,543 bill, with Zhang owing $500 copays.(Laura Buckman for KFF Health News)
Some free-standing emergency rooms may look like urgent care centers but come with ER charges. Tieqiao Zhang believed he was visiting urgent care when he twice sought treatment for a kidney stone at a facility called an “urgent care emergency center.” The visits yielded a $19,543 bill, with Zhang owing $500 copays.(Laura Buckman for KFF Health News) Amari Vaca was 3 months old and recovering from surgery when he contracted the virus RSV, or respiratory syncytial virus. He was transferred by air ambulance, but his insurer denied the claim, determining it wasn’t medically necessary. His mother, Sara England, recently said their appeal failed. They owe $97,000.(Kevin Painchaud for KFF Health News)
Amari Vaca was 3 months old and recovering from surgery when he contracted the virus RSV, or respiratory syncytial virus. He was transferred by air ambulance, but his insurer denied the claim, determining it wasn’t medically necessary. His mother, Sara England, recently said their appeal failed. They owe $97,000.(Kevin Painchaud for KFF Health News) A couple of months before transition surgery, the hospital contacted Wren Vetens with a higher estimate than expected and offered a discount if she paid upfront — which she did. When she got a bill, Vetens told her insurer she had contacted “Bill of the Month.” She received a refund.(Lauren Justice for KFF Health News)
A couple of months before transition surgery, the hospital contacted Wren Vetens with a higher estimate than expected and offered a discount if she paid upfront — which she did. When she got a bill, Vetens told her insurer she had contacted “Bill of the Month.” She received a refund.(Lauren Justice for KFF Health News)The Resolution
Some bills signal that there’s more to be done to tame a health care industry in which seemingly everything can be billable. Mansi Bhatt took her toddler, Martand, to the emergency room for a burn on his hand, but after a long wait, they left before being seen by a doctor. Just checking in yielded an $859 bill, which the family had to pay since they hadn’t met their deductible.
Even new protections, such as those for air-ambulance bills, have problems. Amari Vaca was 3 months old and recovering from open-heart surgery when he contracted the life-threatening virus RSV, or respiratory syncytial virus. When doctors said he needed specialized care, he was transferred by air ambulance to a different hospital. The family’s insurer denied the claim, determining the flight wasn’t medically necessary, and the hospital declined to file an appeal. Vaca’s mother, Sara England, notified KFF Health News in October that their final appeal was denied. They owe $97,000.
And old bills die hard. When “Bill of the Month” reconnected with Phil Gaimon this fall, he said he had called his providers recently to check his outstanding balance — and learned it was, at last, zero.
 Phil Gaimon was competing to qualify for the Olympics when he was in a bicycle crash and wound up with bills topping $200,000. He recently learned his outstanding balance is zero. “I think I was home from the hospital in 10 days, riding my bike again in a month,” he says. “And then the bills … three years.”(Heidi de Marco/KFF Health News)
Phil Gaimon was competing to qualify for the Olympics when he was in a bicycle crash and wound up with bills topping $200,000. He recently learned his outstanding balance is zero. “I think I was home from the hospital in 10 days, riding my bike again in a month,” he says. “And then the bills … three years.”(Heidi de Marco/KFF Health News)Gaimon was competing to qualify for the Olympics when he was in a bicycle crash and wound up with bills topping $200,000. “I think I was home from the hospital in 10 days, riding my bike again in a month,” he said in an interview. “And then the bills … three years.”
While our “Bill of the Month” partnership with NPR is sunsetting, the “Bill of the Month” series will continue as KFF Health News investigates your medical bills. Keep them coming! And watch for future stories in The Washington Post’s Well+Being.
Elisabeth Rosenthal is a senior contributing editor for KFF Health News and the creator of “Bill of the Month.”
Emily Siner reported the audio story.
Henry Larweh and Molly Castle Work of KFF Health News contributed reporting for this article.







![Paleo Cranberry Orange Bread [grain-free + no added sugar]](https://i0.wp.com/healthyhelperkaila.com/wp-content/uploads/2020/05/CranberryOrangeBreadFeatured.png?fit=1501%2C1501&ssl=1)

![Healthy Peanut Butter Banana Protein Pancakes [dairy-free + gluten-free]](https://i0.wp.com/healthyhelperkaila.com/wp-content/uploads/2024/11/PBBananaPancakesFEATURED.png?fit=1531%2C1536&ssl=1)








 English (US) ·
English (US) ·