In an Advil study about pain experiences, 74% of Black people said there is bias in how their pain is diagnosed and treated. Quána Madison has had more than her share of medical issues over the last decade. After learning in 2015 that she was at high risk for developing several aggressive forms of cancer, Madison underwent a hysterectomy, double mastectomies, and an oophorectomy to remove her ovaries, all so she could live a healthy, long, normal life.
Three months later, she experienced several complications, including necrosis of her remaining breast tissue and vaginal cuff dehiscence. This rare but potentially life-threatening tear can happen after a hysterectomy. After barely surviving that experience in 2017, Madison was diagnosed with fibromyalgia, autoimmune disease, chronic pain syndrome, chronic fatigue syndrome, and a host of other maladies, including anxiety and depression.
An Awful Encounter At An Emergency Room
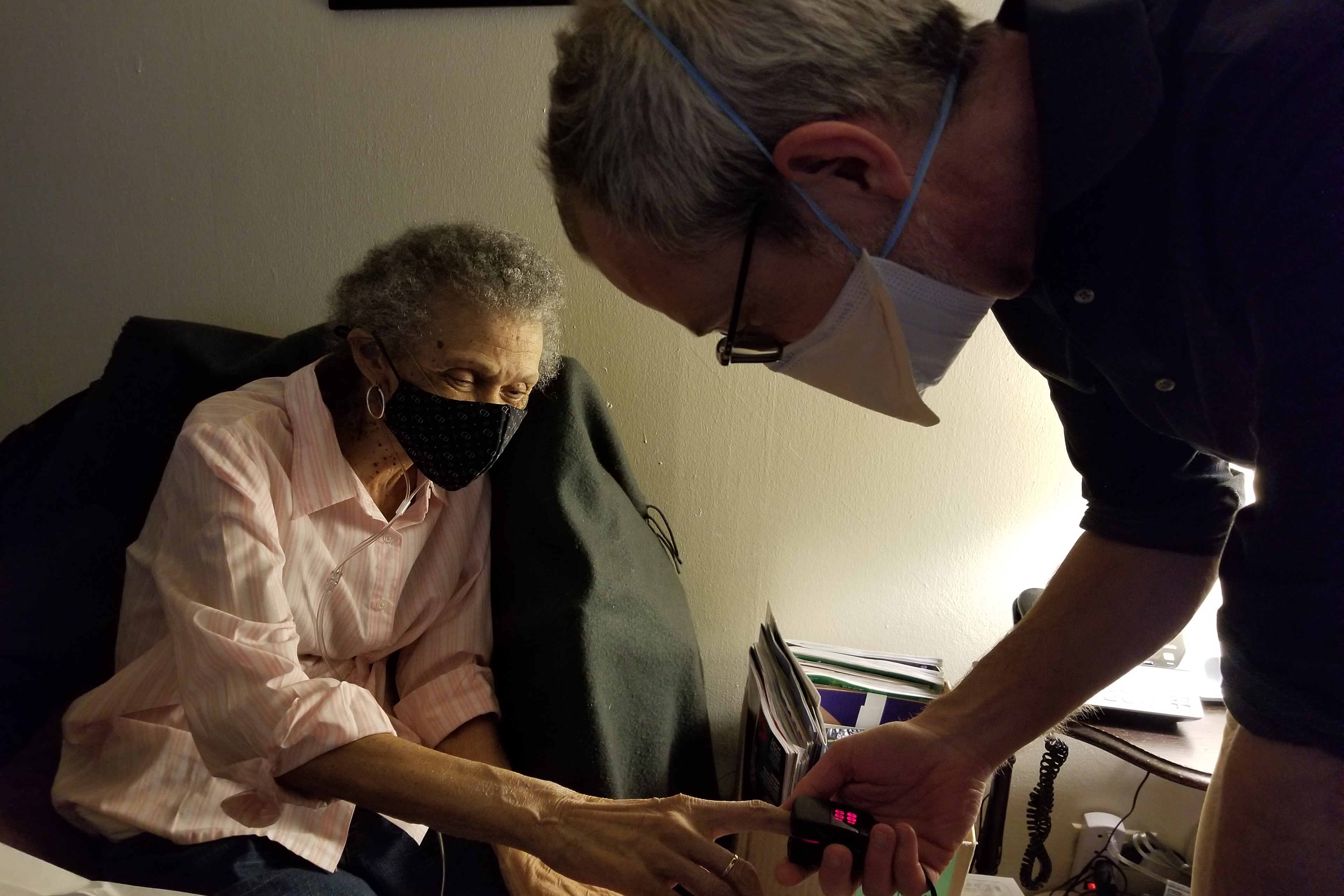
Her conditions forced her to drop out of her doctoral program, which resulted in the multi-disciplinary artist also losing her health insurance. Nonetheless, Madison sought help at a local emergency room when she started to feel excruciating pain in her legs, leaving her unable to walk. While in triage, a nurse attempted to take her blood to try to figure out what was going on.
“I explained that I had several chronic pain conditions that made getting a blood draw more hypersensitive and that I had small, rolling veins,” explains the 43-year-old.
“When she kept missing my vein, and I would have a response, she grabbed my arm even harder and told me, ‘That doesn’t hurt you.’
The situation escalated once Madison took out her phone to record the encounter, a practice she says she has done before because “I’ve learned that I’m not believed unless I have evidence.” Madison recounts the nurse becoming so outraged that she reached over her body to grab the phone away, and that’s when she was told, “You’re just trying to get pain drugs. You’re a drug seeker.”

Soon after, the nurse called the police. If it wasn’t for her husband (who is white and was in the room with her), an officer (who happened to be a person of color), and a calmer E.R. doctor, Madison firmly believes that she would have been arrested that day.
“That experience left me feeling dehumanized, fearful to seek care, traumatized, and depressed because people think I don’t experience pain.”
Who Started the Black People Don’t Feel Pain Narrative?
Although it may seem like Madison’s story is the extreme, it’s not. There is a long history in the United States of pain inequity, where Black patients do not receive adequate measures to properly and fairly assess and treat their pain symptoms. In the 19th century, a wealthy white plantation owner and respected physician, Dr. Thomas Hamilton, did his best to prove that Black bodies functioned differently than white bodies, namely that Black skin was, in fact, “thicker” and thus more impervious to pain. Hamilton’s experiments were inhuman and influential enough to lead to many other obnoxious fallacies based on racist ideologies.
In 1840, Dr. James Madison Sims performed obstetric and gynecological procedures on several enslaved girls and women in Alabama without anesthesia while his colleagues observed and took notes. These theories may have been constructed centuries ago, but they are still perpetuated today by practicing healthcare professionals of varying backgrounds.
Dr. Uché Blackstock is the founder and CEO of Advancing Health Equity and the author of “Legacy: A Black Physician Reckons with Racism in Medicine.” In her book, she recounts her experience of receiving a false diagnosis during her first year of medical school. After her third visit to the E.R., she was treated for an emergency appendectomy and infection resulting from a rupture.
Dr. Blackstock says she understands racial bias in medicine from both patient and physician perspectives.
“I was told I didn’t seem to be in that much pain,” says Dr. Blackstock. “It’s an experience that Black patients and other patients of color often have when they seek care for an issue that involves pain, and they feel like they are not listened to, and their concerns are minimized, or they’re simply just dismissed.”
The Believe My Pain Project
Dr. Blackstock has partnered with the Advil Pain Equity Project, a multi-year collaboration with Morehouse School of Medicine and BLKHTH, to review the impact of racial bias in pain management. Several Black patients shared their personal stories of having an underlying diagnosis that was either missed or delayed, resulting in both emotional and physical harm. The testimonials, while frustrating, also allow room for hope.
Morehouse School of Medicine is offering two new courses to educate the next generation of doctors on how to better treat Black patients in pain.
Conversations have already started with other medical schools to follow suit. Plus, Black patients are encouraged to learn new ways to better advocate for themselves with the tools they can access at believemypain.com.
In a recent study, Advil surveyed 2,000 Americans and found that 83% of Black people said they have had a negative experience seeking help managing pain. “The numbers were overwhelmingly reinforcing that the Black community was where we needed to lean in and help drive awareness and make a difference as it relates to Black pain and Black inequities,” said Stacey Harris, vice president of marketing U.S. Pain & Rx to OTC Switch at Haleon, the consumer health care company that produces Advil.

In Pain Alone On a Gurney For Eight Hours
Chelsea Parker is optimistic that the Advil Pain Equity Project will make a difference in how she and other Black patients are treated in the future. Parker was diagnosed with sickle cell disease at three years old and has found ways to manage the rollercoaster of physical and emotional pain that comes with her condition. Now, the 31-year-old social worker knows what to expect when in crisis.
The excruciating cramps in her joints, mainly her thighs and legs, and sometimes in her chest, can be overwhelming.
This was the case in August 2024 when her brother drove her to her local emergency room in Michigan. Instead of receiving care, she was ignored and left alone on a gurney in the hallway for nearly eight hours. “I would see a nurse or doctor now and again, but they didn’t give me water, an IV, or any fluids and eventually only offered me two milligrams of pain medication,” said Parker.
“I fell asleep, and when I woke up, I was down on the other side of the hallway. No one asked how I was doing or if I was ok.”
Parker claims it wasn’t until her mother and mentor arrived that she felt like her symptoms were finally addressed. Nonetheless, she doesn’t plan ever to return there. The next time she’s in crisis, she’d rather travel to a hospital further away. “They could have had more compassion for what I was going through,” says Parker. “Even though they can’t see it, I was showing that I was in pain. And yet, it didn’t matter.”
The Truth, Reconciliation, Healing & Transformation Research Project
In addition to the Advil Pain Equity Project, the American Medical Association (AMA), one of the oldest and most influential professional organizations for physicians and the science of medicine, has teamed up with the Harvard Kennedy School’s Institutional Antiracism and Accountability (IARA) Project for the “Truth, Reconciliation, Healing, and Transformation” (TRHT) Archival Research Project. For the first time, the AMA will fully open its records from the last 177 years for historians to scrutinize the historical roots of racial disparities, hoping that doing so will lead to groundbreaking policies and changes in medicine.
Research Associate Ángel Rodriguez. is leading part of the project under Professor Khalil Gibran Muhammad, founder and director of the IARA Project. “We’re very excited to take the next 24 months to do something no one has done before,” says Rodriguez. “It’s also important that our scholarship reflects the highest quality and rigor of our analysis to include real evidence to back up what we will ultimately share. We want to be able to make specific insights and recommendations.”
Rodriguez is confident that the TRHT Archival Research Project will help explain why some health inequities persist today.
The team wants to create a deeper understanding and context around some of these disparities based on historical evidence, which will lead to changes in policies and practices that better protect Black patients in pain.
Boldly stated, American medical personnel have failed Black patients in many ways. Healing has to come from both sides. The burden isn’t just on the patients to advocate for themselves; it’s also on the healthcare system to change how doctors do medicine.
Patient-centric care is a start where physicians, nurses, and others can use more inclusive language with Black patients that unpacks medical jargon and acknowledges that Black patients can be the experts of their own experiences.
The hardest part, however, may be for practitioners to finally acknowledge their own implicit bias and internalized negative beliefs about Black people. Look at how those beliefs impact the way they diagnose and treat patients. Maybe only then can we treat pain fairly for everyone, regardless of race.
Wendy L. Wilson is an award-winning journalist who has written for BET.com, theGrio.com, Ebony Magazine, Jet Magazine, and Essence Magazine.

















 English (US) ·
English (US) ·