Your skin is home to hundreds of types of bacteria that make up the skin microbiome. One of these bacteria is called staphylococcus aureus, or staph. It’s usually harmless, but can sometimes cause an infection.
Staph infections can range from mild, where they’re easily treated with antibiotics, to more severe and even life threatening. Because one staph infection can look very different from another, it’s important to identify the cause of a suspected infection.
Learn more, including what symptoms to look out for, complications that can happen and when it may be time to see a doctor for treatment if you think you may have a staph infection.
What is a staph infection?
Staphylococcus, or staph, is the name of a group of bacteria commonly found on your skin, and for around 30% of people in the U.S., in the nose. Most commonly, staph infections are caused by a specific staph bacteria in that group called Staphylococcus aureus.
A staph infection begins when staph bacteria enters your body, usually through a cut or an open sore. The severity of the infection depends on certain risk factors, the strength of the bacteria, where you’re infected and how treatable it is.
Staph can infect a number of places in the human body, including both on and in your:
- Skin
- Blood
- Bones
- Heart
- Lungs
- Muscles
Are staph infections contagious?
Yes, staph infections are contagious and typically spread through skin-to-skin contact with a person who has an infection. Pus from an abscess is particularly contagious, but it can also be spread through:
- Shared items, like towels or toothbrushes
- Surfaces that are frequently touched (depending on the surface material, the bacteria can live for days, weeks and even months outside the body)
- Food handling
- Poor hygiene
- Droplets from coughing and sneezing, but this is rare
Staph infection symptoms depend on where you’re infected
Staph infections can cause a number of visible symptoms, but they can also cause other symptoms that aren’t as easy to detect, depending on where and how you’re infected. When you’re infected on your skin, it’s usually obvious that you have a staph infection. But when staph infects other areas of your body, it can cause you to experience general flu-like symptoms that can be easily mistaken for something else.
Staph infections on the skin most commonly occur on the face around the mouth and nose. Usually, they start with a small area of the skin and look like a pimple or a blister that can be swollen, red and warm to the touch. But they can cause other conditions, including:
- Folliculitis – When hair follicles become inflamed due to staph, pimple-like blisters form under the follicles and cause pain. This can occur anywhere on the body where there’s hair, and most commonly occurs due to sweating or skin being rubbed.
- Impetigo – A common skin rash in children, staph bacteria can cause red, itchy sores usually on the face, arms and legs. The sores fill with pus, break open and leave a yellow crust on the skin. Impetigo is highly contagious, but usually very treatable if caught early.
- Abscesses and boils – These are the most common symptoms of staph infections. An abscess is a contagious, painful, pus-filled sore that forms under the skin. And a boil is a painful red bump that develops in an oil gland or hair follicle. These can occur anywhere on the skin, but are most common in areas that have hair, sweat or friction, including the face, neck, armpits, thighs and genital area.
- Cellulitis – This is an infection that forms and can spread under the skin, where the infected area gets hot, swollen and looks red. It can happen for a variety of reasons, including from human, animal and insect bites, skin ulcers caused by diseases like diabetes, and from cracked and peeling skin anywhere on the body.
- Styes – Common in children, staph bacteria can cause a bump near the eye that’s warm, red and uncomfortable. Most styes go away with at-home treatment like a warm compress on the eye or over-the counter stye medication, but some require antibiotic treatment.
- Staphylococcal scalded skin syndrome – This typically affects babies and small children under six years old due to underdeveloped or compromised immune systems. Staph bacteria can cause skin to peel off over large parts of the body, making skin look like it’s been burned or scalded. And like impetigo, it’s highly contagious, but easily treatable and usually goes away a few days after beginning treatment.
Staph infections can occur in other areas of the body
If a staph infection occurs in the body besides the skin, it can cause other health conditions that range from mild to life threatening, including:
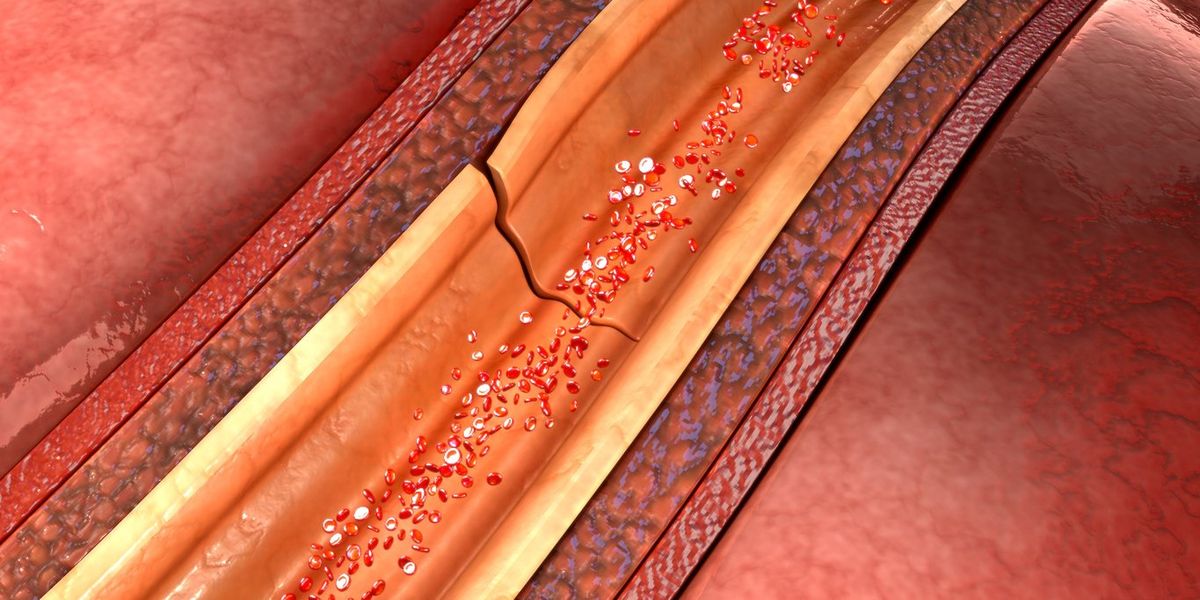
- Blood poisoning – Also known as septicemia or bacteremia, staph bacteria can enter the blood stream and cause a fever, difficulty breathing, elevated heart rate, mental confusion and dangerously low blood pressure.
- Bone infections – Staph bacteria can cause osteomyelitis, where bacteria can enter your bones due to severe puncture wounds, broken bones, or after a surgery. It can cause pain and swelling, as well as chills and fever.
- Endocarditis – This is a serious, potentially life-threatening heart condition where bacteria can reach the heart valves through the bloodstream. It can cause fever, weight loss, rapid heart rate and sweating.
- Food poisoning – Staph bacteria can be ingested when eating, usually when food is improperly handled or stored. This can cause the typical symptoms of food poisoning, like nausea, vomiting and diarrhea. In most cases, this resolves on its own without treatment.
- Mastitis – This is a breast infection that commonly occurs in people who are breastfeeding. Staph bacteria enter the skin, usually through a cracked nipple, and can lead to inflammation, pain and occasionally abscesses.
- Pneumonia – Staph bacteria can infect the lungs, causing fever, chills, difficulty breathing, chest pain and a general unwell feeling. If left untreated, it can lead to complications like sepsis, where the immune system doesn’t respond properly to an infection, or bacteremia, which is bacteria in the bloodstream.
- Toxic shock syndrome (TSS) – TSS usually occurs during menstruation with the use of tampons, but it can also happen after surgery, with a soft-tissue infection or due to burns on the skin. It’s a more severe form of blood poisoning, and can cause fever, muscle aches and a rash. It can also become life threatening if not promptly treated.
- Urinary tract infection (UTI) – UTIs are commonly caused by a form of staphylococcus bacteria called Staphylococcus saprophyticus, which can resolve without treatment. Staphylococcus aureus can also cause a UTI, but it’s rare, can be life threatening, and typically requires treatment.
Risk factors for staph infections
Anyone can get a staph infection, but there are groups of people who are at higher risk. In particular, people who work in hospitals and care facilities tend to have more staph bacteria on their skin, but other risk factors include:
- Staying in a hospital or care facility for an extended period of time
- Being on kidney dialysis
- Breastfeeding
- Having an open cut or sore
- Being in close contact with someone who is infected
- Having a weakened immune system
- Having a chronic condition, like diabetes
- Having a medical device inside your body, like an artificial joint or a catheter
- Using tampons for prolonged periods of time
- Using injectable drugs
How a staph infection is diagnosed and treated
Your doctor will begin by assessing your symptoms and taking a sample from the infected site, or a blood or urine sample. The sample will be tested to see if it’s positive for staph.
Based on the results, they’ll determine a course of treatment. This usually means getting antibiotics in pill form, intravenously (IV), or through a prescription topical antibiotic. They may also drain, clean and dress your wound, if you have one.
Depending on the severity of the infection, you may have to stay in the hospital for treatment where you’ll stay in an isolated area to avoid spreading the infection to others.
Methicillin-resistant staphylococcus aureus (MRSA) and staph infections
MRSA and staph infections are the same thing, but MRSA is a more severe form of staph infection that’s resistant to certain antibiotics. Antibiotic-resistant MRSA is the result of long-term, unnecessary antibiotic use. But even when antibiotics are used properly, they can still contribute to the problem.
Treatment for MRSA may require a course of antibiotics that is stronger than typically used, usually given through an IV. But in some cases, antibiotics may not be necessary, and doctors will drain the boil or abscess to treat the infection.
Most MRSA infections occur in people who have been in hospitals or other medical facilities, like nursing homes or dialysis centers. Others occur in people who have had invasive surgeries or medical device implantations. MRSA infections in these situations usually occur due to accidental contamination or lapses in the sterile protocols that health care workers and facilities typically follow closely.
MRSA infections can also occur among healthy populations. This is called community-associated MRSA. It usually begins as a skin boil, and is spread through person-to-person contact. It’s most commonly found in places where people live in crowded conditions, child care facilities and in contact sports, like wrestling.
Prevention is important when it comes to staph infections
Proper handwashing can prevent a lot of things, and it’s especially important when it comes to staph infections and stopping the spread of bacteria. Other hygiene tips include:
- Using hand sanitizer with a concentration of between 60-80% alcohol when you’re not able to wash your hands right away
- Cleaning cuts and scrapes immediately and covering them with a clean bandage
- Avoiding contact with other people's wounds or bandages, and wearing gloves if contact can’t be avoided
- Draining your breasts fully at each feeding or pumping session if you’re breastfeeding
- Avoiding sharing personal items such as towels, washcloths, razors or clothing
- Keeping your home environment clean by ensuring all surfaces are regularly disinfected, including countertops, doorknobs and light switches
- Changing tampons regularly (if you use them) and using the lightest absorbency needed for your flow
If you think you have a staph infection, it’s important to see your doctor
While minor staph infections can clear up on their own, there’s no guarantee that will be the case. For your health, it’s best to get treatment and use antibiotics as prescribed so the infection won’t get worse and spread to other areas of your body, and to stop the infection from coming back.
For minor conditions caused by staph like mastitis or a UTI, you can make an appointment with your primary care doctor, try an urgent care video visit or visit Virtuwell, our convenient online clinic.
But if you have a severe skin infection, experiencing symptoms that won’t go away on their own, or experiencing concerning symptoms, go to the nearest urgent care or emergency room as soon as possible. It’s important to get treatment right away, so the infection doesn’t have a chance to spread and become worse.


















 English (US) ·
English (US) ·