Facial volume loss, skin laxity, and textural change are common concerns with aging. Many patients seek gradual, credible improvement that preserves natural contours. Sculptra™ offers a collagen-stimulating approach that emphasizes tissue quality over time rather than instant volumization.
Clinical choices should align with patient goals, anatomy, and risk tolerance. For procedural planning and context, clinicians can review clinical product information for Sculptra 2 vials and consider how a biostimulatory strategy fits into a broader treatment plan.
What Collagen Stimulation Aims to Address
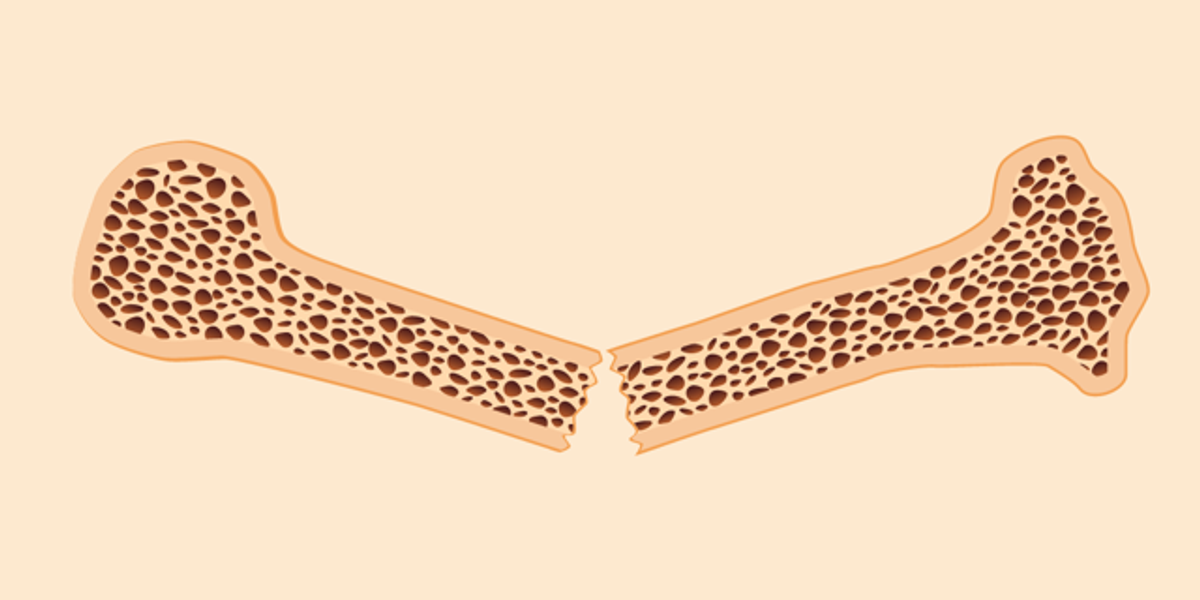
Age-related facial changes reflect bone remodeling, fat compartment shifts, and dermal thinning. Patients describe hollowing in the temples, midface flattening, and skin creasing. Lifestyle factors, weight cycling, sunlight, and illness can accelerate these features.
Biostimulatory treatments target dermal and subdermal support by promoting new collagen formation. Rather than filling a line, the intent is to improve structural integrity and skin quality. This trajectory usually requires a series of sessions and patience with the remodeling timeline.
How Poly-L-Lactic Acid Works
Poly-L-lactic acid (PLLA) acts as a biostimulatory implant. The particles trigger a controlled fibroplastic response, increasing collagen over several months. As the carrier fluid dissipates, the scaffold effect emerges gradually.
Compared with hyaluronic acid gels, PLLA does not provide immediate bulk. Instead, it builds subtle tissue support with progressive changes. Patients should understand that outcomes evolve and may require maintenance once a baseline is achieved.
Patient Selection and Expectation Setting
Ideal candidates tolerate a gradual timeline and value natural, low-key change. They often present with diffuse volume loss, mild to moderate laxity, or textural decline. Candidates should maintain stable weight and healthy skin care, as fluctuations affect predictability.
Screen for contraindications and cautions. These include active infection, inflammatory skin disease in the treatment area, poor wound healing, pregnancy, or breastfeeding. Discuss history of autoimmune conditions, keloids, or prior granulomatous reactions. Set expectations about multiple sessions, delayed onset, and maintenance scheduling.
Anatomy, Planning, and Layer Selection
A focused facial mapping clarifies priorities and safety boundaries. Evaluate bony landmarks, fat pad support, and skin thickness. Identify zones where biostimulation benefits quality and lift, and where it provides limited return.
Depth and distribution influence outcomes. Deep structural support may benefit the temple and lateral face, while more superficial planes can influence skin quality in select regions. Avoid high-risk areas and respect vascular anatomy. When in doubt, plan conservatively and reassess after collagen remodeling.
Session Structure and Treatment Course
Most patients need a series of sessions spaced weeks apart. The number of sessions varies by age-related volume deficit, metabolic factors, and treatment zones. Reassessment between visits allows calibration and prevents overcorrection.
Coordination with other modalities is common. Biostimulation can pair with neuromodulators for dynamic lines or device-based skin tightening for laxity. Staging therapies helps minimize compounded swelling and clarifies each modality’s contribution.
Safety Profile and Risk Mitigation
Adverse events range from transient swelling and bruising to delayed nodules and rare granulomas. Risk reduction starts with proper reconstitution, appropriate plane selection, gentle technique, and conservative volumes per site. Massage protocols, if used, should be tailored and explained clearly to the patient.
Promptly address asymmetry, persistent edema, or textural irregularities. Distinguish among edema, bruising, and palpable product. Delayed-onset nodularity requires systematic evaluation, including consideration of biofilm and inflammatory etiology. Establish and document a follow-up pathway to manage evolving findings.
Aftercare and Patient Guidance
Patients should anticipate mild swelling, tenderness, and possible bruising in the first days. Intermittent cold compresses and head elevation may reduce early swelling. Encourage a short period of reduced strenuous activity and alcohol intake to limit exacerbated edema.
Clear instructions support adherence. If you recommend massage, give frequency and duration guidance; otherwise, instruct patients to avoid manipulating treated areas. Encourage sun protection to support collagen health and reduce post-inflammatory dyschromia in sensitive patients.
Integrating with Other Injectable Strategies
Collagen stimulators complement immediate volumizers when used judiciously. Hyaluronic acid products can refine specific contours while PLLA improves broader support and quality. Consider sequencing to reduce confounders in both safety and aesthetics.
For colleagues reviewing options across categories, the Dermal Fillers category provides context for agents that deliver more immediate volumization. Strive for a cohesive plan that aligns product characteristics with regional anatomy and patient priorities.
Special Populations and Considerations
Thinner skin phenotypes can show textural improvement but may reveal irregularities if planes are superficial. In high-mobility regions, use caution to avoid visible surface change or nodularity. Patients with significant photodamage may benefit from adjunctive resurfacing or device therapies after biostimulation consolidation.
Immunologic history and prior filler exposure warrant careful discussion. Long-interval follow-ups help monitor late changes and maintain trust. Documentation should include lot tracking, treatment maps, volumes per site, and post-care instructions.
Practical Counseling Points
• Set a 3–6 month horizon for visible remodeling, with staged assessments.
• Emphasize that collagen quality and lift are the goals, not instant projection.
• Review common transient effects and signs that warrant earlier contact.
• Align home care with barrier support and photoprotection to sustain gains.
• Time other procedures to minimize compounded inflammation and confounders.
Measuring Outcomes
Standardized photography at each visit provides objective comparison. Include neutral lighting and consistent head position. Palpation notes on tone and thickness add qualitative context to visual changes.
Patient-reported outcomes matter. Ask patients to rate changes in skin quality, makeup application, or facial fatigue appearance. These perspectives often capture benefits beyond simple volumetric metrics.
Summary and Takeaways
Sculptra™ can support gradual, natural-appearing facial rejuvenation by encouraging collagen deposition. Success depends on thoughtful selection, conservative planning, and careful follow-up. The modality fits best for patients who value incremental improvement and sustained tissue quality.
Integrate collagen stimulation within a comprehensive plan that addresses movement, volume, and skin health. Reinforce sun protection and steady lifestyle habits to preserve results. Strong documentation and predictable aftercare pathways reduce risk and improve satisfaction.
Medical disclaimer: This content is for informational purposes only and is not a substitute for professional medical advice.
For institutional resources, policies, and product categories, visit MedWholesaleSupplies . Maintain your own clinical standards and consult evidence-based protocols when tailoring treatment plans.
Isreal olabanji a dental assistant and public health professionals and has years of experience in assisting the dentist with all sorts of dental issues.
We regularly post timely and trustworthy medical information and news on Fitness, Dental care, Recipes, Child health, obstetrics, and more.









![Healthy Single-Serve Peanut Butter Protein Cookie [vegan + gluten-free]](https://i0.wp.com/healthyhelperkaila.com/wp-content/uploads/2025/06/PBCookie5.png?fit=800%2C800&ssl=1)









 English (US) ·
English (US) ·